I Learned ACLS to Save Lives
I’ll never forget my first day as a nurse. A patient suddenly stopped breathing, and my heart raced. I knew Advanced Cardiovascular Life Support (ACLS) could help. It’s a system that saves lives during heart emergencies. In this article, I’ll explain what are the elements of a system of care ACLS in simple words. You’ll learn how it works, why it matters, and how to use it. Whether you’re new or experienced, I’ll share tips and stories to make it clear. Let’s dive into this life-saving system!
What Is a System of Care in ACLS?
ACLS helps doctors and nurses save people during heart emergencies. A system of care is how we organize people, tools, and steps to make this happen. It’s like a team working together to win a game. The system ensures everyone knows their job and acts fast. It’s built to improve patient survival and recovery. According to the American Heart Association, a strong system can double survival rates for cardiac arrest.
The Four Key Elements of an ACLS System
A system of care in ACLS has four main parts. These are structure, process, system, and patient outcomes. Each part is like a piece of a puzzle. Together, they create a plan to save lives. Let’s break them down in simple terms.
Structure: The Building Blocks
Structure is the foundation of ACLS. It includes people, tools, and training.
- People: Trained nurses, doctors, and paramedics who know ACLS.
- Tools: Defibrillators, heart monitors, and airway devices.
-
Training: Classes to teach CPR and emergency steps.
For example, in my hospital, we check defibrillators daily to ensure they work. This keeps us ready for emergencies.
Process: The Steps We Follow
Process means the rules and steps we use. These are called protocols. They tell us what to do, like giving CPR or medicines. For instance, if someone’s heart stops, we follow a clear plan: check the pulse, start CPR, and use a defibrillator. Protocols make sure everyone acts the same way, which saves time. I once saw a team save a patient by following these steps perfectly.
System: Working Together
The system is how all parts connect. It’s like a team passing a ball to score a goal. Hospitals, ambulances, and communities work together. For example, paramedics start CPR, then hand the patient to the hospital team. This teamwork helps patients recover faster. A strong system also tracks data to improve care.
Patient Outcomes: The Goal
Patient outcomes are the results we want. This means helping people survive and recover. A good ACLS system improves survival rates and quality of life. For example, quick CPR can help someone wake up and go home healthy. I’ve seen patients thank our team after surviving a heart attack. That’s why we focus on outcomes.
The Chain of Survival: A Simple Guide
The Chain of Survival is a key part of ACLS. It’s a set of steps to save someone whose heart stops. There are two chains: one for out-of-hospital cardiac arrest (OHCA) and one for in-hospital cardiac arrest (IHCA). Here’s how they work.
Out-of-Hospital Chain of Survival
This chain helps people outside hospitals, like at home or a park.
- Call for Help: Spot a heart emergency and call 911.
- Start CPR: Push hard and fast on the chest.
- Use a Defibrillator: Shock the heart to restart it.
- Advanced Care: Paramedics give medicines and oxygen.
-
Hospital Care: Doctors provide recovery care.
I once saw a bystander start CPR at a park. It kept the patient alive until paramedics arrived.
In-Hospital Chain of Survival
This chain is for hospitals. It starts with watching patients closely.
- Watch for Problems: Check vital signs like heart rate.
- Call for Help: Alert the emergency team.
- Start CPR: Begin chest compressions.
- Use a Defibrillator: Shock the heart if needed.
-
Recovery Care: Monitor in the ICU.
In my hospital, we caught a patient’s weak pulse early. Quick action saved their life.
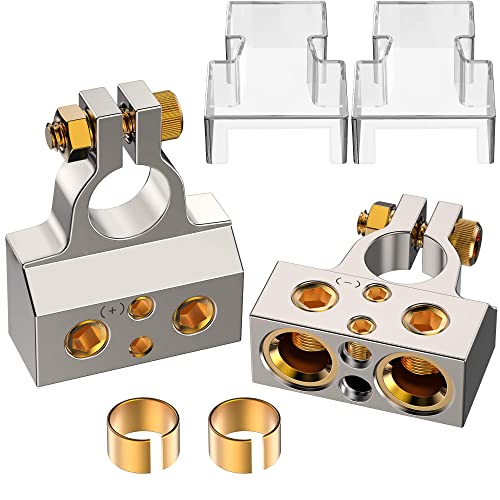
Tools You Need for ACLS
ACLS needs special tools to work well. Here’s a simple list:
- Defibrillator: Shocks the heart to restart it.
- Heart Monitor: Shows heart rhythm.
- Airway Tools: Help patients breathe.
-
Medicines: Like epinephrine to help the heart.
These tools must be checked daily. Once, a broken defibrillator delayed our team. Now, we double-check everything.
Table 1: Common ACLS Tools
Caption: A quick look at tools used in ACLS.
| Tool | What It Does | Example Use |
|---|---|---|
| Defibrillator | Restarts heart with a shock | Shock for irregular rhythm |
| Heart Monitor | Shows heart activity | Check pulse during CPR |
| Airway Device | Helps patient breathe | Insert tube for oxygen |
Steps to Build a Strong ACLS System
Creating a good ACLS system is like building a house. You need a plan and practice. Here are three easy steps:
- Train Everyone: Teach nurses and doctors ACLS skills.
- Check Equipment: Make sure tools work every day.
-
Practice as a Team: Run drills to stay ready.
I run practice drills monthly. It feels like a game, but it prepares us for real emergencies.
Benefits and Challenges of ACLS Systems
ACLS systems save lives, but they have pros and cons.
Benefits
- Faster Response: Quick action saves more people.
- Better Teamwork: Everyone knows their job.
- Improved Recovery: Patients go home healthier.
Challenges
- Cost: Tools and training can be expensive.
- Time: Practice takes effort and planning.
-
Stress: Emergencies are intense for teams.
I’ve felt the stress of a cardiac arrest, but training makes it easier to stay calm.
Table 2: Benefits vs. Challenges
Caption: Comparing the pros and cons of ACLS systems.
| Aspect | Benefits | Challenges |
|---|---|---|
| Response Time | Saves lives quickly | Needs constant practice |
| Equipment | Reliable tools help | Expensive to maintain |
| Teamwork | Clear roles improve care | Training takes time |
My Tips for ACLS Success
After years in healthcare, I’ve learned a few tricks. Here are my top tips:
- Stay Calm: Take a deep breath before acting.
- Know Your Role: Understand your job in the team.
-
Practice Often: Drills make actions automatic.
Once, I forgot a step during a drill. Practicing more helped me get it right in a real emergency.
Visual Ideas for Better Understanding
To make ACLS clearer, try these visuals (not included):
- Chain of Survival Diagram: Show steps for OHCA and IHCA.
- Tool Guide: Picture of a defibrillator and heart monitor.
- Team Roles Chart: List who does what in an emergency.
Common Mistakes to Avoid
Mistakes can happen in ACLS. Here are three to watch for:
- Skipping Equipment Checks: Always test defibrillators.
- Poor Communication: Speak clearly to your team.
-
Ignoring Training: Practice keeps skills sharp.
I once saw a team struggle because they skipped a drill. Don’t make that mistake!
Continuous Improvement in ACLS
ACLS systems get better with feedback. After every emergency, we review what worked and what didn’t. This is called Continuous Quality Improvement (CQI). For example, we found our team needed faster communication. Now, we use a checklist to stay organized. CQI helps us save more lives.
Table 3: Improving ACLS with CQI
Caption: How feedback makes ACLS better.
| Step | Action | Result |
|---|---|---|
| Review | Discuss what went wrong | Find weak spots |
| Train | Practice new skills | Improve team response |
| Update Tools | Fix broken equipment | Ensure tools work |
Conclusion
ACLS systems of care are like a superhero team for heart emergencies. They combine people, tools, and steps to save lives. The four elements—structure, process, system, and patient outcomes—work together for success. Whether you’re a nurse or just curious, you can learn ACLS basics. Try practicing CPR or joining a training class. Visit the American Heart Association for free resources. Share your thoughts in the comments—have you seen ACLS in action? Let’s keep learning to save lives!
Frequently Asked Questions
What Are the Elements of a System of Care ACLS?
The elements are structure, process, system, and patient outcomes. Structure includes people and tools, like defibrillators. Process means following steps, like CPR protocols. System is teamwork across hospitals and ambulances. Patient outcomes focus on survival and recovery. Together, they ensure fast, effective care.
Why Is ACLS Important?
ACLS saves lives during heart emergencies. It teaches teams to act fast with CPR, defibrillators, and medicines. A strong ACLS system improves survival rates. For example, quick CPR can help someone recover fully. It’s critical for hospitals and paramedics.
What Tools Are Needed for ACLS?
ACLS uses defibrillators, heart monitors, airway tools, and medicines like epinephrine. These tools help restart hearts and keep patients breathing. Always check equipment daily to avoid delays. I’ve seen a broken monitor cause confusion, so testing is key.
How Does the Chain of Survival Work?
The Chain of Survival is steps to save someone in cardiac arrest. For out-of-hospital, it’s calling 911, CPR, defibrillation, advanced care, and recovery. In hospitals, it starts with watching patients, then CPR and ICU care. Each step saves lives.
What’s the Difference Between BLS and ACLS?
Basic Life Support (BLS) is simple CPR and defibrillation. ACLS adds advanced steps like medicines and airway tools. BLS starts care, while ACLS continues it for complex cases. Both are vital, but ACLS needs more training.
How Can I Learn ACLS?
Take an ACLS course from the American Heart Association or National Healthcare Provider Solutions. Classes include hands-on practice and videos. I took a course and practiced drills. It’s fun and builds confidence for emergencies.
What Are Common ACLS Mistakes?
Common mistakes include skipping equipment checks, poor team communication, and ignoring training. Always test tools like defibrillators. Speak clearly during emergencies. Practice drills to stay sharp. I’ve seen teams improve after fixing these errors.